We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Date published : 17 November, 2022 Date last updated : 16 August, 2024 Download as a PDFVersion 1, 17 November 2022
High-quality patient records are the foundation of good clinical care delivery. Delivering safe and efficient patient care depends on having high quality patient records and, therefore, the right information available when clinical decisions are made. New models of care delivery mean that records are of high quality and that they are also fit for sharing.
Organisational boundaries between health and care providers are becoming increasingly blurred as technology is used to share patient and health information. Patients increasingly have access to their full (historical and prospective) GP record online. Digital communication, digital consultation and digital monitoring of conditions are now fully integrated elements, well established elements of healthcare delivery.
High-quality electronic records contain all the information needed about a patient’s health to provide good care to that person. This information can be relied upon to make clinical decisions with confidence when it:
Missing, inaccurate, or non-standard information can, however, lead to Inconsistent care, or risk the quality, and safety, of care delivered.
It is important to remember that most health professionals are not data experts and that the link between poor data quality and its effects on patient care are not always easily appreciated. This is especially true as the purpose becomes more distant from direct care, the original purpose for which most information is collected in a GP patient record. In research and population health management, for example, care needs to be taken interpreting this information as the data may not have been originally collected for that purpose.
This guidance is aimed at helping to understand the importance of record quality.
The main purpose of a patient record, whether handwritten or digital, is to support direct patient care. Other uses, e.g. for population health management, research and for legal reasons, are secondary.
Clinical records must be clear, complete, accurate, up-to-date, and legible. All clinicians are required to keep high quality records that meet these standards so that they can be used for the various purposes of:
There is another article in this series on the purpose of the GP electronic health record which covers the topic in more detail.
This guidance focuses on records which are primarily composed during the direct care of the patient. Non-clinical purposes and secondary uses in modern general practice systems are almost completely dependent on the quality of the data captured as part of direct care. Most of this data is captured by health care professionals interacting with their GP IT system.
The representation of health data is complex, but it needs to fulfil the purpose for which it is being considered. Understanding the various purposes of health records can help define what a high-quality health record consists of. It is, however, important to remember that the primary purpose of the record is to support the individual care of the patient. It is unlikely that a record will fulfil all purposes equally, and often there is a trade-off to be considered.
The meaning of what previously may have been described as a high-quality record has changed dramatically over the years. Before the introduction of GP IT systems, a good quality record may have been considered succinct documentation regarding a patient interaction, diagnosis and plan written intelligibly on handwritten notes. In an era of rapid technological advancement and highly connected systems, the definition of a high-quality record is now more complicated.
It is also important to remember that patient record systems contain a variety of clinical and non-clinical data from demographics, administrative, correspondence, clinical interactions, etc. It must also go further to capture context and in a modern-day general practice IT system, providing a conduit by which health professionals can communicate, interact, and record decisions. The quality of the record must be defined in the context for which it is used.
The record must also be in a format that facilitates the sharing of information across organisational boundaries.The ability to share patient information from the health record is becoming an ever-increasing demand on the GP health records generally.
A high-quality record, therefore, needs to:
Clinical data quality has multiple dimensions and ultimately the data needs to be fit for purpose. The Government Data Quality Hub has extensive guidelines on how data quality is assessed. There are other definitions, but Annex A to this article has a more complete overview and outline of the dimensions of data quality with respect to patient records.
From a more practical perspective, ensuring record quality in current GP IT systems can be achieved by:
Whilst coding can increase the machine-readable element of a record, free text can provide detailed narrative content and context that cannot be captured using coded entries alone. High quality records are often a mixture of free text (which contain complex narrative and easily human readable) and coded data.
Below is a simple example of how coding improves data quality.
Consider the simple entry of a patient’s weight and height. These can be entered as free text into a consultation, the BMI can be calculated independently and then added. This is shown below:
The entry shown is simply free text and does reflect certain characteristics. Whilst this is generally human readable and outlines the values of weight, height, and BMI there are, however, a number of problems:
The example below is the same information entered against specific SNOMED CT codes. The information is almost identical.
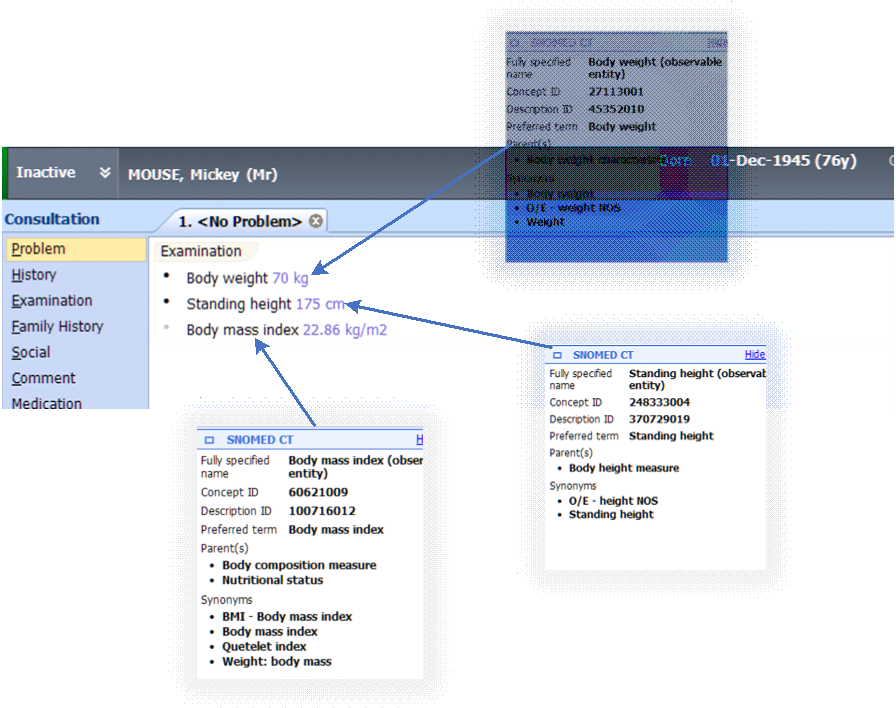
This example highlights how the coding can improve the record quality from so many perspectives. These improvements are:
The example here of the coded vs uncoded entry whilst simple, highlights the power of coding in improving the quality and utility of patient records. Coding is perhaps the single most important method of improving health care records and ensuring they are fit for purpose.
When sharing records, it is critical that both systems understand the terminology. Having a standardised coding terminology such as SNOMED CT ensures that information can be transferred, and understanding is retained. When local, system specific codes are used, however, the meaning may be lost when transferred.
The GP record’s primary purpose is to capture information about the consultation or encounter. As stated previously, free text can capture important context as readable narrative but may not be in a form that can be easily coded. Having high quality coded information accompanying the clinical context and patient narrative is vital to improve the utility of the record. It also allows the record to be computer readable and processed depending on the purpose. Most clinical information is captured as an encounter or problem. In order to understand how this affects record quality and how it is maintained, it is important to understand what encounter based and problem-based records are.
Encounter-based GP records typically contain information relating to a single episode or encounter relating to:
They can also contain a multitude of other information including but not limited to:
An encounters problem can be defined in many ways and varies from system to system.
The above encounter-based record needs to be linked to a problem and, in turn, a problems list which persists between encounters.
Problem orientation consists primarily of:
The problem itself is typically defined as a recognised SNOMED code. This can be accompanied by variety of attributes such as episode descriptors (First Episode, Review, Flare up, etc) significance, active, duration.
Different system suppliers use these attributes differently, so it is important to ensure you understand how these can be utilised. Often, however, some of these attributes don’t have well-defined states, for example major/minor significance of problems are not clearly defined and need to be considered in the context of the problem itself.
General practice records are primarily problem-orientated and encounter-based, but when there is a sequence of encounters, the GP record can become a powerful longitudinal clinical record of a particular problem. All these problems form the problem list. How well this clinical information is maintained and organised will vary from practice to practice and clinician to clinician. The problem list can provide a powerful summary of a patient’s past and present conditions that may be relevant to their care or that particular encounter.
The way problem lists are displayed and managed also vary, based on the clinical system, and it’s important to become familiar with this functionality. Current clinical systems also have several other features that enhance the problem list by allowing users to navigate to any documents, medications, or referrals, linked to a particular problem or SNOMED CT code.
The key to a high-quality problem list is that it encompasses all those aspects of data quality outlined in Annex A (namely that it is complete, accurate, relevant, accessible, and timely). This will involve an element of curation from the clinical staff maintaining the problem list.
Most system providers have several methods to maintain the quality of the problem list. These include changing the status/descriptor of a problem, ending a problem, grouping problems, combining problems, evolving problems, deleting problems.
Some examples of the evolution and development of a problem list over time can be found in the PRSB and Royal College of Physicians (RCP) Guidance for recording problems and diagnoses in electronic health records.
There are more advanced aspects of problem-orientated records management, including linking documentation or entities such as documents, referrals, and medication to problems. Other facilities include categorising problems by significance, length of problem activity, priority. Some systems even have the ability to nest, merge and cluster problems. These advanced features can aid and improve record quality but do vary based on GP system supplier, so please contact your supplier for further details.
Records should not be amended except in one of a few circumstances, for example when:
If record content is incorrect then it should be corrected. Modern health record systems allow deletion or amendment of the content whilst keeping a clear audit trail of what has been amended. It is also good practice, and most GP IT systems allow for, a free text note of the reasons for the amendment or deletion, with the date and time of the change. Clearly, correcting a record helps improve its quality.
Clinical patient data is considered special category data under the UK General Data Protection Regulations (GDPR) and Data Protection Act 2018. This dictates that patients should be allowed the right to rectification of inaccurate personal data without undue delay.
There may be occasions when a patient’s record is not available, for example:
A full set of notes should be taken, including any discussion of history, medications, etc., and added to the full record at the earliest opportunity. A note of the reasons for the record not being available should be included. The record should be coded appropriately when access is available to the GP IT system.
The following is a summary of the characteristics of high-quality data (CARAT) as suggested by organisations such as PRIMIS:
1. Complete | Data can be considered complete when all the required data for a particular purpose is present and available to be used. Completeness relates to determining that the patient’s record has all diagnoses, allergies, vaccinations, operations, or events present within the record. Consider a patient record with missing allergy information. The consequences of this could be profound, and the omission clearly constitute an incomplete record.
Completeness for an individual patient could reflect that it contains all the relevant codes for all diagnoses, allergies, vaccinations, operations, or events. Across a population it means that all patients with a particular condition diagnosed have it correctly coded in all the records.
2. Accurate | This is when the data reflects reality or a genuine real-world occurrence. Accuracy can be quite challenging as it can change over time and is, therefore, difficult to monitor. An example may be a patient that presents with chest pain and is coded as such. At that point in time there is no clear cause for the chest pain, and this is, therefore, an accurate reflection in the data. That diagnosis may, however, change from chest pain to myocardial infarction following further investigations. Uncertain symptoms can become certain diagnoses.
Recording a diagnosis of stroke based on clinical symptoms and then later being it being proved not to be the case would render the initial diagnosis inaccurate and would need evolving/correcting.
This highlights the transient nature of accuracy especially when the diagnosis is uncertain and also the importance of maintaining and evolving problems.
3. Relevant | When considering data quality, relevance implies there is a reason to collect or record the information in the patient record. You must consider whether you really need this information, and for what purpose. Relevant data is usually closely linked to the purpose for which it is being collected. For example a diabetic review might record blood pressure as this is relevant in the context of diabetes. Recording the patient’s temperature in the record during the diabetic review would not, however, be relevant as it adds nothing to the diabetic review and is unrelated to diabetes in this context.
4. Accessible | Data may be recorded completely and accurately, but if we cannot extract information that we need this can been seen as an accessibility issue. Accessibility describes how easy it is to retrieve the required information as and when it is needed. Coded data is typically more accessible than free text and can be displayed and organised in various ways by the GPIT system as the codes themselves are understandable to the system. With modern GPIT systems there can also be vast qualities of information being drawn into the record from multiple sources, how this information is organised and coded can aid accessibility.
5. Timely | Data that is available when expected and when needed is timely. The purpose determines what would be considered timely. In the context of a clinical interaction, most professional bodies consider the contemporaneous entry of medical information as one of the most important aspects of healthcare. Contemporaneous entry of clinical information also supports the other aspects of data quality including accuracy and completeness.